By breathing, the lungs are in direct contact with the environment and, thus, also with pathogens and pollutants, such as tobacco smoke. With the immune system, the body has several ways to ward off these negative influences. Neutrophils play an important role in the immune defense. They are the most common subtype of white blood cells. Their task is to ward off bacterial and viral pathogens as well as fungi. They are also involved in the development of inflammatory reactions. If there is a strong and uncontrolled activation of neutrophils, however, it can lead to tissue damage and eventually diseases.
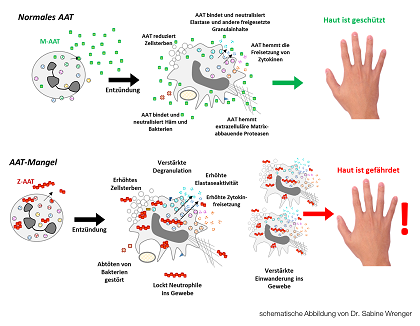
Alpha-1-antitrypsin is crucial for the regulation of neutrophils and protects the body during immune defense against endogenous substances. During an inflammatory reaction, neutrophils themselves produce the protective protein alpha1-antitrypsin (AAT). For immune defense, they also release cytokines and elastases to ward off unwanted invaders in the body, e.g. in the lungs. However, this immune defense is nonspecific and must be tightly regulated so that it does not damage the body's own cells. In healthy individuals, AAT helps prevent neutrophils to cause an overshooting immune response. Reduced secretion or loss of function of AAT, such as hereditary AAT deficiency, may result in uncontrolled neutrophil over-activity.
AAT deficiency manifests primarily in the lungs. Due to the gradual loss of the alveoli, an pulmonary emphysema develops. People with hereditary PiZZ antitrypsin deficiency have an increased risk for emphysema development and cigarette smoking further increases this risk. Lack of AAT results in an increased accumulation and activity of neutrophils in these patients, eventually leading to lung tissue damage.
Although AAT deficiency predominantly manifests in the lungs, the reduced regulation of the immune response of neutrophils may also cause inflammation of other organs, e.g. the skin (see picture). The so-called neutrophilic panniculitis is a localized inflammation of the subcutaneous fat tissue. The diagnosis of this rare disease is complicated by the fact that the different types of panniculitis are very similar in their clinical picture. Mostly, panniculitis is a nonspecific erythema caused by dilated blood vessels, such as sunburn or inflammation.
In the known cases of neutrophilic panniculitis caused by AAT deficiency, middle-aged women (30-60 years) carried the ZZ genotype in 70 percent of the cases. However, neutrophilic panniculitis also occurs in carriers of the MS, SS, MZ and SZ genotype. So far, it is not certain if the relation to these genotypes is accidental or significant. The pathogenesis of AAT deficiency-related panniculitis is still largely unexplained. However, it is well recognized that an increased neutrophil activity as a result of AAT deficiency leads to disease development. In fact, several patients with ATT deficiency and panniculitis have been successfully treated with AAT replacement therapy.
Neutrophils also play a role in various other chronic inflammatory skin diseases, such as psoriasis. Although psoriasis is well characterized clinically and histologically, its origin is unclear in detail. However, some cases of AAT deficiency associated with psoriasis have already been reported. Among the patients with severe psoriasis an increased number of the AAT genotypes MS, MZ and SS was found.
Neutrophils largely regulate the properties and functions of the skin. The role of AAT deficiency in the development of skin diseases is just beginning to be understood.
Text: BREATH / CD, S. Janciauskiene
Figure: Sabine Wrenger