On 16.01.2020 the German Parliament opposed the opt-out solution for organ donation endorsed by the German Federal Minister of Health, Jens Spahn. Therefore, the current system of consent given during lifetime remains. Prof. Dr. Axel Haverich, Head of the Transplant Center at Hannover Medical School (MHH), also argued for the opt-out solution. Prior to the parliamentary decision, he said that „the medical possibilities of organ transplantation are so well developed that we could help many more people if there were sufficient donor organs available“. Since the willingness to donate still remains at a low level and, after the parliamentary decision no changes are to be expected, other ways must be found to help patients who urgently need a donor organ.
Prof. Dr. Haverich, Head of the Clinic for Cardiac, Thoracic, Transplant and Vascular Surgery (HTTG), and Prof. Dr. Gregor Warnecke, Transplant Surgeon at the HTTG, therefore participated in the EXPAND Study, that looked into the improvement of donor lungs using the Organ Care System (OCS) Lung.
Currently, only about 20% of the donor lungs from brain-dead organ donors are actually used for transplantation. The remaining 80% do not fulfil the strict requirements for donor organs. Due to the overall low number of donor lungs and the number of these donor organs actually used, about 30% of the patients on the waiting list are denied the lifesaving transplant. Due to their deteriorating health status, 15% can no longer be operated on and are crossed off the list, while a further 15% die before a suitable organ can be found.
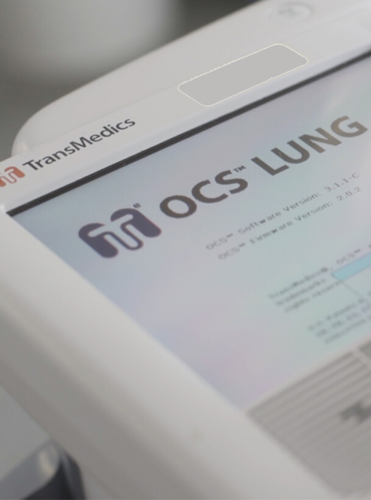
In various studies, it has already been shown that the quality of donor organs can be significantly improved if these undergo artificial respiration and ventilation during transport from the donor to the recipient. Inpatient systems for this type of care are already established in some clinics. The portable OCS Lung facilitates continuous organ function from the time of removal right up to the point of transplantation. This possibility prompted the transplantation experts to examine whether donor lungs, that otherwise do not meet the stringent criteria for transplants, could be considered for transplantation using the OCS Lung.
Six clinics in the USA, one clinic in Belgium and the MHH participated in this project. Together, they defined extended inclusion criteria for the EXPAND Study, according to which otherwise excluded organs should be utilized for transplantation using the OCS Lung. Amongst these are donated organs from deceased cardiovascular donors and brain-dead donors who are over 55 years old and exhibit an ischemic time, i.e. the time of hypoperfusion of the organ, of a maximum of six hours. For this study, 93 donor lungs could be found, of which 81 complied with the transplantation criteria. Sixty-six of the 79 lungs that could ultimately be implanted came from the USA and had, on average, been previously declined by 35 clinics due to the stringent criteria. After removal, the donor lungs were connected to the OCS Lung and rinsed there continuously with a special solution, supplied with oxygen at a rate of ten breaths per minute and with a steady flow of blood. The lung function was checked after removal and again prior to transplantation in the recipient.
After transplantation, various parameters of the transplant recipients were observed, e.g. the development of a primary graft dysfunction (PGD), acute pulmonary insufficiency or survival after 30 days, 6 months and 12 months. As reference values, data were used from the INSPIRE Study, that carried out similar studies with donor lungs that, on the other hand, met the standard criteria. Seventy-eight of the 79 transplanted patients survived the first 30 days, 74 the first 6 months and 72 the first 12 months. These results correspond to those also achieved by the INSPIRE Study. Rejection reactions in the EXPAND Study were even observed in fewer cases than in the INSPIRE Study. Only the occurrence of PGD syndromes was increased. In future, use of certain operative methods could counteract this aspect. Currently, data on the long-term development of transplant patients are being collected.
Comparison of donor lungs, selected on the basis of the expanded criteria and supplied via the OCS Lung, with donor organs meeting previous criteria, shows that more organs than previously could be transplanted with the OCS Lung. Patients would then spend less time on the waiting list, which is not only preferable from a medical viewpoint. The shorter waiting time also brings with it massive financial savings, which can also balance out the cost of an OCS Lung for the clinics. If more lungs become available in the future as donor organs through the use of the OCS Lung, this could signify a revolution in lung transplantation.
Text: BREATH/AB
Photo: BREATH
Original publication: Loor, G., Warnecke, G., Villavicencio, M. A., Smith, M. A., Kukreja, J., Ardehali, A., Hartwig, M., Daneshmand, M. A., Hertz, M. I., Huddleston, S., Haverich, A., Madsen, J. C., Van Raemdonck, D. Portable normothermic ex-vivo lung perfusion, ventilation, and functional assessment with the Organ Care System on donor lung use for transplantation from extended-criteria donors (EXPAND): a single-arm, pivotal trial Lancet Respir Med 2019 Aug; : doi: 10.1016/s2213-2600(19)30200-0.

Prof. Dr. Axel Haverich with the OCS Lung