Extracorporeal Membrane Oxygenation
The function of a damaged lung can be supported temporarily by the use of so-called extracorporeal membrane oxygenators (ECMO). These ECMOs are made up of a fine mesh net of hollow fiber membranes in which an oxygen/gas mixture flows. On the outside of these hollow fibers, the patient’s blood flows past, whereby it is finally oxygenated and decarboxylated by diffusion. However, the period of clinical application is limited to a few weeks, as there is an increase in thrombocyte adhesion on the membrane surface as well as deposition of fibrin aggregates even after just a few days, which finally lead to a loss in function of the ECMO. Quite often, formation of a bacterial biofilm is observed on these surfaces. The complement system is then activated with subsequent leukocyte adhesion and secretion of inflammatory mediators, that can cause life-threatening sepsis.
These facts highlight the urgent need to develop a lasting usable lung replacement procedure, which is the target of Prof. A. Haverich’s working group.
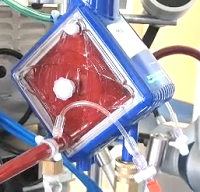
Based on the functional principles of commercially available ECMO systems, a completely intracorporeally implantable biologically compatible biohybrid lung should be developed.
Initially, the blood compatibility of the gas exchange membranes should be improved, as well as their resilience with regard to formation of biofilm. To that end, the side of the hollow fiber membranes in contact with the blood is covered with an endothelial monolayer. In addition to the physiological anti-thrombogenic function of the endothelial cells, these should also inhibit the binding of proteins and bacteria and thus preventatively counteract the development of biofilm.